Should beta-blockers be
discontinued
when a patient is
admitted to the
hospital with
acutely decompensated
heart failure?
June 2006 | Volume 73 | Number 6 | Pages 557-559
| Wassim H. Fares, MD Department of General Internal Medicine, Cleveland Clinic |
Ashish Aneja, MD Department of General Internal Medicine, Cleveland Clinic |
Return to One-Minute Consult Index
Data on this topic are scant. However, most experts recommend discontinuing beta-blockers in patients with shock and lowering the dose for those with bradycardia or hypotension.1 All others should continue to receive a beta-blocker at the same dose they had been receiving.
Furthermore, the evidence clearly supports resuming (or starting) a beta-blocker after the patient attains a euvolemic state before he or she leaves the hospital unless a clear contraindication exists.2–4
Start or resume a beta-blocker after a euvolemic state is attained, before hospital discharge
Beta-Blockers: The Standard for Chronic Heart Failure
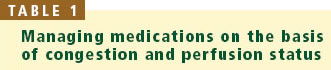
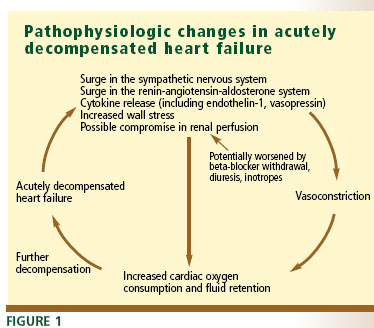
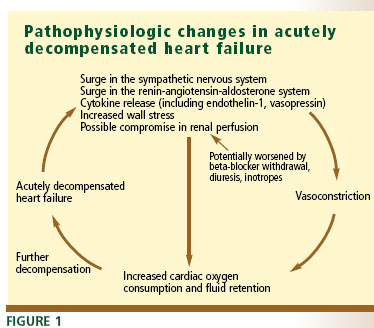
Beta-adrenergic antagonists—specifically, metoprolol succinate
(extended release) and carvedilol, the only agents of this class approved
for this indication—are the standard of care for chronic heart failure
because they have been proven to decrease mortality rates.5–7 They should also be beneficial in acutely decompensated heart failure
because they help break the neurohormonal vicious circle that occurs in
both conditions (FIGURE 1).
Crude mortality rates of patients after a first hospitalization for acutely decompensated heart failure are 11.6% at 30 days and 33% at 1 year.8 Brief periods of treatment with medication during the initial presentation of acutely decompensated heart failure may significantly affect long-term survival.9
However, there are very few data on the efficacy and safety of continuing beta-blockers in patients admitted to the hospital with acutely decompensated heart failure.
The question has not
been directly tested: an appropriate clinical trial would be difficult
to design, and it would be difficult to recruit patients in acute decompensation
to such a study.10 Consequently, the balance of risks
(negative inotropic effects) and benefits (inhibiting the adverse effects
of the sympathetic nervous system) of beta-blocker therapy has not been
established in acute decompensation.
The uncertainty has led to inconsistent management: some physicians discontinue these drugs until the patient is close to euvolemic status, some reduce dosage, and others continue the patient’s outpatient regimen.
Patients with more severe symptoms of heart failure have more side effects
at the start of beta-blocker therapy than those with milder disease.11 But one cannot assume that patients sick enough to be admitted to the
hospital will not tolerate beta-blocker therapy: the hemodynamics of acutely
decompensated heart failure differ from those of chronic severe heart
failure. In fact, patients with severe symptoms (New York Heart Association
[NYHA] class IV) on beta-blockers have a significantly lower mortality
rate than comparable patients not taking beta-blockers.5,6 In addition, abruptly withdrawing beta-blockers in patients with heart
failure results in clinical deterioration and should be avoided.12–14
Recommendations

Figure 2 is an algorithm to help guide decisions regarding beta-blockers for patients with acutely decompensated heart failure, based on vital signs and perfusion status. It assumes that the patient has been on a stable dose of a beta-blocker for at least a few weeks before being hospitalized. Again, we emphasize that a patient who is not already taking a beta-blocker should be started on one once he or she is in a compensated, euvolemic state, before leaving the hospital.2–4
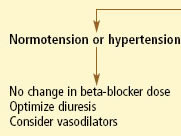
A comparable and practical approach for the overall pharmacologic management of patients with acutely decompensated heart failure is based on the patient’s congestion and perfusion status Table 1.

In patients with adequate perfusion, every effort should be made to avoid
reducing or stopping beta-blockers. Evidence indicates that beta-blockers
can be continued in patients with worsening heart failure without
compromising safety.15,16
Patients with shock, bradycardia, or hypotension. Most experts recommend discontinuing beta-blockers in patients with shock and reducing the dosage for those who have bradycardia or hypotension.1 Treatment with diuretics should be optimized, and inotropes should be considered. Hemodynamic monitoring is recommended.
In patients with recurrent decompensation, briefly holding beta-blockers or significantly lowering the dose may be warranted (unless inappropriate therapy is to blame).
Patients with documented significant worsening of left ventricular ejection fraction may benefit from a reduction of the beta-blocker dose, although the evidence to support this practice is weak,14 and it could deprive patients of the full benefit of the drug, especially if they are doing well clinically.5–7
Inotropic agents. The routine use of inotropic agents is not recommended. However, for patients receiving a beta-blocker who need an inotropic agent because of low cardiac output, hypotension, or cardiogenic shock, a phosphodiesterase inhibitor such as milrinone is preferable to a betaadrenergic agonist such as dobutamine or dopamine because phosphodiesterase inhibitors work at a site distal to beta-adrenergic receptors.1,17–19
Acknowledgment: The authors thank Dr. Randy C. Starling, Dr. Christopher O. Phillips, and Dr. Franklin Michota for their valuable input.
References
- Nieminen MS, Bohm M, Cowie MR, et al; ESC Committe for Practice Guideline (CPG). Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology. Eur Heart J 2005; 26:384–416.
- Tarantini L, Cioffi G, Opasich C, et al. Pre-discharge initiation of beta-blocker therapy in elderly patients hospitalized for acute decompensation of chronic heart failure: an effective strategy for the implementation of beta-blockade in heart failure. Ital Heart J 2004; 5:441–449.
- Fonarow GC, Abraham WT, Albert NM, et al. Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF): rationale and design. Am Heart J 2004; 148:43–51.
- Gattis WA, O’Connor CM, Gallup DS, Hasselblad V, Gheorghiade M; IMPACT-HF Investigators and Coordinators. Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure: results of the Initiation Management Predischarge: Process for Assessment of Carvedilol Therapy in Heart Failure (IMPACT-HF) trial. J Am Coll Cardiol 2004; 43:1534–1541.
- The Cardiac Insufficiency Bisoprolol Study II (CIBIS II): a randomised trial. Lancet 1999; 353:9–13.
- Effect of metoprolol CR/XL in chronic heart failure: Metoprolol
CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999; 353:2001–2007. - Packer M, Coats AJ, Fowler MB, et al; Carvedilol Prospective Randomized Cumulative Survival Study Group. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651–1658.
- Jong P, Vowinckel E, Liu PP, Gong Y, Tu JV. Prognosis and determinants of survival in patients newly hospitalized for heart failure: a population-based study. Arch Intern Med 2002;162:1689–1694.
- Silver MA, Horton DP, Ghali JK, Elkayam U. Effect of nesiritide versus dobutamine on short-term outcomes in the treatment of patients with acutely decompensated heart failure. J Am Coll Cardiol 2002; 39:798–803.
- Poole-Wilson PA. Treatment of acute heart failure: out with the old, in with the new. JAMA 2002; 287:1578–1580.
- Macdonald PS, Keogh AM, Aboyoun CL, Lund M, Amor R,
McCaffrey DJ. Tolerability and efficacy of carvedilol in patients with New York Heart Association class IV heart failure. J Am Coll Cardiol 1999; 33:924–931. - Swedberg K, Hjalmarson A, Waagstein F, Wallentin I. Adverse effects of beta-blockade withdrawal in patients with congestive cardiomyopathy. Br Heart J 1980; 44:134–142.
- Waagstein F, Caidahl K, Wallentin I, Bergh CH, Hjalmarson A. Long-term beta-blockade in dilated cardiomyopathy. Effects of short- and long-term metoprolol treatment followed by withdrawal and readministration of metoprolol. Circulation 1989;80:551–563.
- Lechat P, Escolano S, Golmard JL, et al. Prognostic value of bisoprolol-induced hemodynamic effects in heart failure during the Cardiac Insufficiency BIsoprolol Study (CIBIS). Circulation 1997;96:2197–2205.
- Gattis WA, O’Connor CM, Leimberger JD, Felker GM, Adams KF, Gheorghiade M. Clinical outcomes in patients on beta-blocker therapy admitted with worsening chronic heart failure. Am J Cardiol 2003; 91:169–174.
- Hunt SA; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 2005; 46:e1–82.
- Shakar SF, Abraham WT, Gilbert EM, et al. Combined oral positive inotropic and beta-blocker therapy for treatment of refractory class IV heart failure. J Am Coll Cardiol 1998; 31:1336–1340.
- Lowes BD, Simon MA, Tsvetkova TO, Bristow MR. Inotropes in the beta-blocker era. Clin Cardiol 2000; 23(3 Suppl):III11–III16.
- Bristow MR, Shakar SF, Linseman JV, Lowes BD. Inotropes and beta-blockers: is there a need for new guidelines? J Card Fail 2001; 7(suppl 1):8-12.